Mental Health and Psychosocial Support for Migrants

Key terms and concepts
Mental health and psychosocial support describe any type of local or outside support that aims to protect or promote psychosocial wellbeing and/or treat mental health conditions. Addressing mental health and psychosocial needs is an integral part of the IFRC’s objective to prevent and alleviate human suffering and protect life, health, and dignity.
Mental health is defined by the World Health Organization as a state of well-being in which every individual realizes his or her own potential, can cope with the normal stresses of life, can work productively and fruitfully, and is able to make a contribution to her or his community.
The term “Psychosocial” refers to the dynamic relationship between the psychological and social dimensions of a person and how these interact. Psychological dimensions include internal emotional and thought processes, feelings, and reactions. The social dimensions include relationships, family and community networks, social values, and cultural practices.
Psychosocial support often taps into existing social networks and relationships, as well as cultural touchstones and shared experiences. For people on the move, these are often missing, which can create additional challenges in coping.
The Movement is committed to ensuring that mental health and psychosocial support is integrated into all services and ongoing programs (Movement MHPSS Policy).

Migration: A stressful experience
Even the easiest, most uneventful migration experience is stressful. Migration involves change, uncertainty and personal risk, while separated from familiar and supportive friends, family, customs and places.
Most migrants visiting HSPs will have had some of the most difficult journeys possible, often witnessing or experiencing traumatic events along the way in addition to having fled stressful or dangerous situations in their countries of origin.
At all phases of the migration journey, migrants will be stressed about money and other means to meet their physical needs, as well as other needs such as continuing education.
A few of the broad categories of stressors that affect well-being during migration include:
Situations experienced in the country of origin are likely to have influenced the decision to leave. These may include conflict or violence, abuse, extreme poverty or loss of livelihood, or other threats to health and well-being.
The hardships associated with the journeys that people have undertaken. This can include the ongoing stress of lack of information, uncertainty, and changing migration policies and routes, as well as hostility, and sometimes exploitation, violence, and abuse.
Difficulties in social and economic inclusion in destination countries or countries of long-term transit, including hostility and xenophobia, and stress-related to asylum applications or other legal processes.

Interviews conducted by the AMiRA programme in West Africa found that the most common stressors reported by migrants included lack of or insufficient funds, health problems, violence, abuse or aggression, worries about family left at home, and fear of failure.
Due to stressors, migrants may:
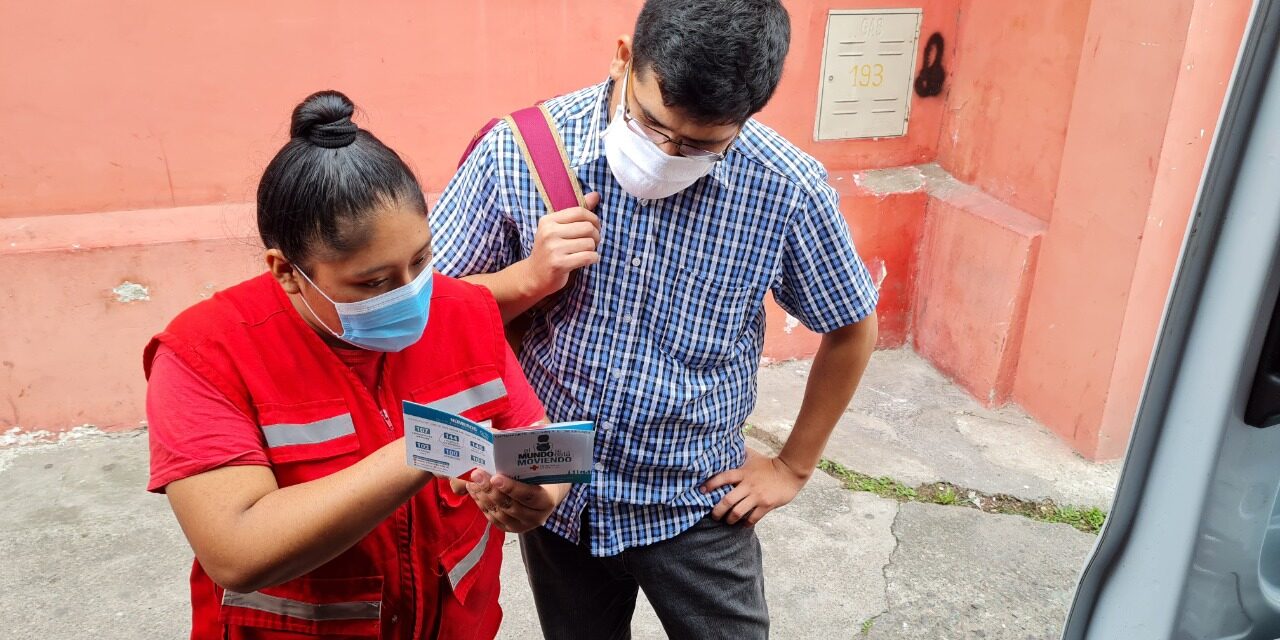
Interventions are relevant/appropriate to an HSP:
Most people show resilience and are able to manage their distress provided that they can activate their personal coping strategies and have access to basic services and external resources -, such as the support of their families, friends, and community.
Challenges
Many migrants face life-threatening situations on their journey and may be exposed to cruel, inhumane, and degrading treatment, including torture. The impact on some people may require specific and long-term mental health interventions impossible or inappropriate to deliver at an HSP.
In fact, it may seem impossible to provide programming at an HSP since migrants often stay only a short time. But virtually any intervention that allows migrants to pause and rest in a place of safety will contribute to their well-being. The process of migration can be very dehumanising, so focus on supports that restore dignity and humanity, and refer for more support where needed and possible.
Every interaction that staff and volunteers have with vulnerable migrants is an opportunity to promote positive mental health and psychosocial well-being.
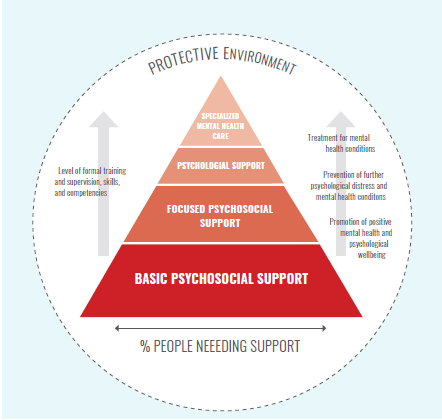
The Movement MHPSS Framework (pyramid) graphic shows different levels of intervention to support mental health and psychosocial wellbeing.
This multi-layered approach does not imply that we must provide services in all layers. However, Movement components are expected to assess, refer and advocate in relation to the full spectrum of mental health and psychosocial support presented in the model. This includes basic psychosocial support through to specialized mental health care.
The layer that is most relevant/appropriate to an HSP is “basic psychosocial support”. This promotes positive mental health and psychosocial wellbeing and resilience. It also promotes social interaction and social cohesion activities within the community.
First layer: Basic psychosocial support activities
- Integrated health, protection, and education sectors
- Accessible to 100% of the affected population
- Psychological first aid
- Awareness-raising on mental health and psychosocial well-being
- Social, sports, and recreational activities
- Safe spaces, particularly child-friendly spaces
- Language, vocational training, or discussion groups
- Activities allow people to relax, connect and build trust
- Particularly activities that do not rely on language and are inclusive.
Think about:
- Where can migrants express concerns or emotions freely? Are there spaces that are private, where people will not be overheard?
- How can services be organised to minimise stress on migrants and maximise their opportunities to relax, rest, and socialise?
- Having an experienced MHPSS delegate to train & support staff and develop MHPSS initiatives.
- Involving migrants in the running of the HSP, especially in information-as-aid initiatives.
The second layer is “focused psychosocial support” with a specific focus on groups, families, and individuals at risk.
- Peer support
- Children’s Resilience Programme
- Support groups for caregivers
- Life skills for youth
- Other group work
The third layer is “psychological support” that includes prevention and treatment activities for individuals and families who present more complicated psychological distress. It is also for people at risk of developing mental health conditions.
Third layer: Psychological support activities
- Counselling
- Psychotherapy
- Activities are usually provided in health-care facilities with accompanying outreach work
- HSPs often will provide referrals to external partners for psychological support
The top layer, “specialized mental health care,” includes specialized clinical care and treatment for individuals with chronic mental health conditions and for persons suffering such severe distress. This is suffering over such a period of time that they have difficulty coping in their daily lives.
Top layer: Specialized mental health care activities
- Treatment centres for survivors of torture
- Alternative approaches to drug therapy
- Services are provided within state health-care and social welfare systems and in detention facilities
Every interaction that staff have with vulnerable migrants is an opportunity to promote positive mental health and psychosocial well-being.
Key points to consider
A safe and dignified environment
A safe and dignified environment is key to supporting people’s mental health and psychosocial well-being, so everything possible must be done to secure that safety. Refer back to the guidance at the beginning of this toolkit on creating a safe environment and, crucially, to the section on safeguarding.
Referral Pathways
Ensure that when you create your referral pathways they include services that respond to the mental health needs of people who may have experienced violence and abuse, as well as services for people with more complex mental health needs.
Training
Staff and volunteers should be trained in psychological first aid, social and recreational activities, and awareness-raising on MHPSS.
Concept Awarness
Investigate how both migrants and volunteers understand the concept of mental health and psychosocial care. There could be cultural stigma connected with the concept, or people may simply not understand them and may hesitate to engage with or reject services entirely.
Key Resources